Red Light Therapy vs Infrared Sauna
Red Light Therapy vs Infrared Sauna — What’s the Difference?
Introduction
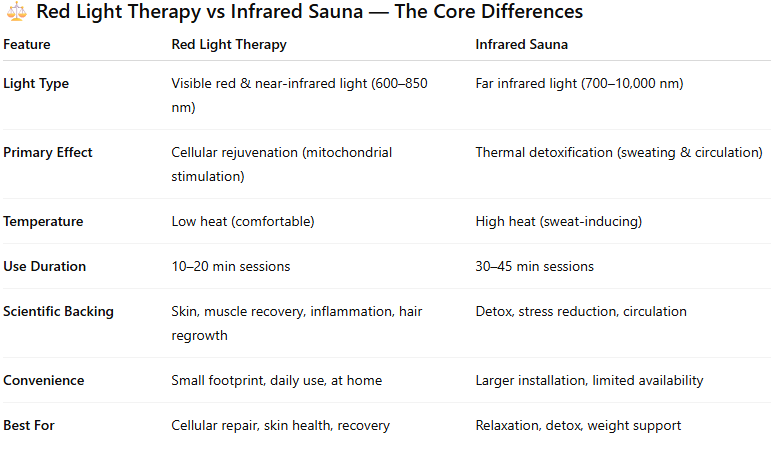
If you’ve been exploring modern wellness tools, you’ve likely come across both red light therapy and infrared saunas. They sound similar — both use light and heat — but they work in fundamentally different ways and deliver distinct health outcomes.
Whether you’re seeking skin rejuvenation, faster muscle recovery, pain relief, or anti-aging support, understanding the difference between the two can help you decide where to invest your wellness budget — or why owning a red light therapy panel may be your smarter long-term move.
What Is Red Light Therapy?
Red light therapy (RLT) — also known as low-level light therapy or photobiomodulation — uses specific wavelengths of red and near-infrared light (typically 630-850 nm) to stimulate cellular energy production (ATP) and promote tissue repair.
Mechanism: Red and near-infrared photons penetrate the skin and are absorbed by mitochondria, the “powerhouses” of your cells, enhancing energy output and reducing oxidative stress.
Goal: Rejuvenate and repair at a cellular level, not just provide surface warmth.
Temperature: Minimal heat; comfortable and safe for daily use.
✅ Clinical support:
Cleveland Clinic confirms RLT “appears safe and effective for improving skin appearance and reducing inflammation.”
UCLA Health notes it may help with “fine lines, loose skin, hair regrowth, and chronic pain.”
PubMed studies show improved wound healing, collagen synthesis, and muscle recovery after consistent use.
What Is an Infrared Sauna?
An infrared sauna uses far infrared (FIR) wavelengths (700–10,000 nm) to heat your body from the inside out rather than heating the air around you.
Mechanism: FIR waves penetrate a few millimeters into the skin, raising core body temperature, inducing sweat, and increasing circulation.
Goal: Detoxification, relaxation, calorie burn, and improved cardiovascular performance.
Temperature: Typically 110–140°F (43–60°C).
✅ Clinical support:
Mayo Clinic reports FIR saunas can “promote relaxation, circulation, and temporary relief from minor aches and pains.”
A 2018 review in Complementary Therapies in Medicine found infrared saunas may support blood pressure reduction and exercise recovery in certain populations.
Science & Safety Comparison
Both methods are non-invasive and safe when used properly.
However, red light therapy offers deeper cellular interaction without raising body temperature, making it ideal for daily, repeatable sessions at home.
Safety Considerations
RLT: Eye protection recommended; minimal side effects.
Infrared sauna: Not suitable for those with heat sensitivity, cardiovascular issues, or dehydration risk.
Both are safe under manufacturer guidelines, but red light therapy offers more targeted, medically supported benefits with lower physical stress.
Which One Delivers Better Results?
It depends on your goals:
For skin rejuvenation, anti-aging, wound healing, and recovery: 👉 Red Light Therapy wins.
For detox, relaxation, and stress reduction: 👉 Infrared Sauna excels.
For overall health optimization: Combine both — use your RLT panel daily, and sauna 1–2× weekly.
But if you’re looking for the highest ROI, minimal maintenance, and scientifically verified benefits, investing in a high-output red light therapy panel gives unmatched versatility.
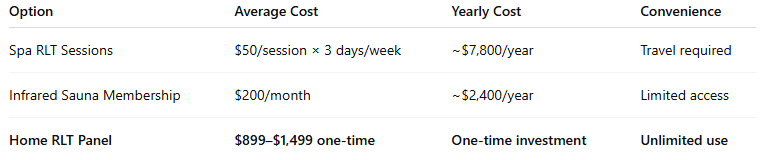
Why Owning a Red Light Therapy Panel Beats Sauna Visits
While saunas are large, costly, and time-intensive, red light therapy panels are:
Compact and suitable for home use
Energy-efficient
Clinically supported
Designed for daily consistency
Cost comparison example:
Owning your own panel delivers unlimited sessions, controlled environment, and long-term savings. Get yours today, here.
Upgrade Your Wellness Routine Today
Ready to experience the science of red light therapy without the sauna’s heat or hassle?
Shop Our Red Light Therapy Panels
Full-body & targeted models
Free shipping to Medford, OR
30-day satisfaction guarantee
Your body’s best light starts here.
FAQ
Q: Can I use red light therapy after an infrared sauna?
Yes — this combo can enhance circulation and recovery, but ensure you hydrate and cool down before starting RLT.
Q: Is red light therapy safer for daily use?
Yes. RLT uses non-thermal light energy and can be used up to 5–7 days/week safely.
Q: Can red light therapy replace an infrared sauna?
For skin, cellular energy, and recovery — yes. For detox and relaxation — a sauna complements RLT.
Check out our most popular blogs on red light therapy to save you time and money on your next purchase with Medford Red Light Therapy:
Scientific References:
Greco M, Guida G, Perlino E, Marra E, Quagliariello E. Increase in RNA and protein synthesis by mitochondria irradiated with helium-neon laser. Biochem Biophys Res Commun. 1989 Sep 29;163(3):1428–1434.
Harris DM. Editorial Comment Biomolecular Mechanisms of Laser Biostimulation. Journal of clinical laser medicine & surgery. 1991;9(4):277–280.
Liu H, Colavitti R, Rovira, Finkel T. Redox-dependent transcriptional regulation. Circ Res. 2005 Nov 11;97(10):967–974.
Huang YY, Chen AC, Carroll JD, Hamblin MR. Biphasic dose response in low level light therapy. Dose Response. 2009;7(4):358–383.
Karu TI, Pyatibrat LV, Kalendo GS. Photobiological modulation of cell attachment via cytochrome c oxidase. Photochem Photobiol Sci. 2004 Feb;3(2):211–216.
Oron U. Light therapy and stem cells: a therapeutic intervention of the future? Interventional Cardiology. 2011;3(6):627–629.
Lane N. Cell biology: power games. Nature. 2006 Oct 26;443(7114):901–903.
Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B. 1999 Mar;49(1):1–17.
Wong-Riley MT, Liang HL, Eells JT, et al. Photobiomodulation directly benefits primary neurons functionally inactivated by toxins: role of cytochrome c oxidase. J Biol Chem. 2005 Feb 11;280(6):4761–4771.
Pastore D, Greco M, Petragallo VA, Passarella S. Increase in <--H+/e- ratio of the cytochrome c oxidase reaction in mitochondria irradiated with helium-neon laser. Biochem Mol Biol Int. 1994 Oct;34(4):817–826.
Karu T, Pyatibrat L, Kalendo G. Irradiation with He-Ne laser increases ATP level in cells cultivated in vitro. J Photochem Photobiol B. 1995 Mar;27(3):219–223.
Basford JR. Low intensity laser therapy: still not an established clinical tool. Lasers Surg Med. 1995;16(4):331–342.
AlGhamdi KM, Kumar A, Moussa NA. Low-level laser therapy: a useful technique for enhancing the proliferation of various cultured cells. Lasers Med Sci. 2012 Jan;27(1):237–249.
Hode L. The importance of the coherency. Photomed Laser Surg. 2005 Aug;23(4):431–434.
Peplow PV, Chung TY, Ryan B, Baxter GD. Laser photobiomodulation of gene expression and release of growth factors and cytokines from cells in culture: a review of human and animal studies. Photomed Laser Surg. 2011 May;29(5):285–304.
Posten W, Wrone DA, Dover JS, Arndt KA, Silapunt S, Alam M. Low-level laser therapy for wound healing: mechanism and efficacy. Dermatol Surg. 2005 Mar;31(3):334–340.
Huang YY, Sharma SK, Carroll J, Hamblin MR. Biphasic dose response in low level light therapy - an update. Dose Response. 2011;9(4):602–618.
Paasch U, Haedersdal M. Laser systems for ablative fractional resurfacing. Expert Rev Med Devices. 2011 Jan;8(1):67–83.
Weiss RA, McDaniel DH, Geronemus RG. Review of nonablative photorejuvenation: reversal of the aging effects of the sun and environmental damage using laser and light sources. Semin Cutan Med Surg. 2003 Jun;22(2):93–106.
Hardaway CA, Ross EV. Nonablative laser skin remodeling. Dermatol Clin. 2002 Jan;20(1):97–111. ix.
Lee SY, Park KH, Choi JW, et al. A prospective, randomized, placebo-controlled, double-blinded, and split-face clinical study on LED phototherapy for skin rejuvenation: clinical, profilometric, histologic, ultrastructural, and biochemical evaluations and comparison of three different treatment settings. J Photochem Photobiol B. 2007 Jul 27;88(1):51–67.
Nanni CA, Alster TS. Complications of carbon dioxide laser resurfacing. An evaluation of 500 patients. Dermatol Surg. 1998 Mar;24(3):315–320.
Sriprachya-Anunt S, Fitzpatrick RE, Goldman MP, Smith SR. Infections complicating pulsed carbon dioxide laser resurfacing for photoaged facial skin. Dermatol Surg. 1997 Jul;23(7):527–535. discussion 535–526.
Sachdev M, Hameed S, Mysore V. Nonablative lasers and nonlaser systems in dermatology: current status. Indian J Dermatol Venereol Leprol. 2011 May-Jun;77(3):380–388.
Dierickx CC, Anderson RR. Visible light treatment of photoaging. Dermatol Ther. 2005 May-Jun;18(3):191–208.
Weiss RA, Weiss MA, Geronemus RG, McDaniel DH. A novel non-thermal non-ablative full panel LED photomodulation device for reversal of photoaging: digital microscopic and clinical results in various skin types. J Drugs Dermatol. 2004 Nov-Dec;3(6):605–610.
Weiss RA, McDaniel DH, Geronemus RG, et al. Clinical experience with light-emitting diode (LED) photomodulation. Dermatol Surg. 2005 Sep;31(9 Pt 2):1199–1205.
Russell BA, Kellett N, Reilly LR. A study to determine the efficacy of combination LED light therapy (633 nm and 830 nm) in facial skin rejuvenation. J Cosmet Laser Ther. 2005 Dec;7(3–4):196–200.
Barolet D, Roberge CJ, Auger FA, Boucher A, Germain L. Regulation of skin collagen metabolism in vitro using a pulsed 660 nm LED light source: clinical correlation with a single-blinded study. J Invest Dermatol. 2009 Dec;129(12):2751–2759.
Abergel RP, Lyons RF, Castel JC, Dwyer RM, Uitto J. Biostimulation of wound healing by lasers: experimental approaches in animal models and in fibroblast cultures. J Dermatol Surg Oncol. 1987 Feb;13(2):127–133.
Kucuk BB, Oral K, Selcuk NA, Toklu T, Civi OG. The anti-inflammatory effect of low-level laser therapy on experimentally induced inflammation of rabbit temporomandibular joint retrodiscal tissues. J Orofac Pain. 2010 Summer;24(3):293–297.
Weiss RA, McDaniel DH, Geronemus RG, Weiss MA. Clinical trial of a novel nonthermal LED array for reversal of photoaging: clinical, histologic, and surface profilometric results. Lasers Surg Med. 2005 Feb;36(2):85–91.
Bhat J, Birch J, Whitehurst C, Lanigan SW. A single-blinded randomised controlled study to determine the efficacy of Omnilux Revive facial treatment in skin rejuvenation. Lasers Med Sci. 2005;20(1):6–10.
Geronemus RG, Weiss RA, Weiss MA, et al. Non-ablative LED photomodulation light activated fibroblast stimulation clinical trial. Lasers Surg Med. 2003;25:22.
McDaniel DH, Newman J, Geronemus R, et al. Non-ablative non- thermal LED photomodulation—a multicenter clinical photoaging trial. Lasers Surg Med. 2003;15:22.
Yu W, Naim JO, Lanzafame RJ. The effect of laser irradiation on the release of bFGF from 3T3 fibroblasts. Photochem Photobiol. 1994 Feb;59(2):167–170.
Schindl A, Heinze G, Schindl M, Pernerstorfer-Schon H, Schindl L. Systemic effects of low-intensity laser irradiation on skin microcirculation in patients with diabetic microangiopathy. Microvasc Res. 2002 Sep;64(2):240–246.
Ben-Dov N, Shefer G, Irintchev A, Wernig A, Oron U, Halevy O. Low-energy laser irradiation affects satellite cell proliferation and differentiation in vitro. Biochim Biophys Acta. 1999 Jan 11;1448(3):372–380.
Weiss RA, McDaniel DH, Geronemus R, et al. Non-ablative, non- thermal light emitting diode (LED) phototherapy of photoaged skin. Laser Surg Med. 2004;16:31.
Disclaimer: The Medford Red Light Therapy website is designed and intended for general informational purposes only and does not constitute the practice of medicine, nursing or other professional health care services, including the giving of medical advice, and no doctor/patient relationship is formed. The use of information on this website is at the user’s own risk. Results may vary by individual. The content of this website is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Users should not disregard or delay in obtaining medical advice for any medical condition they may have and should seek the assistance of their health care professionals for any such conditions.