Does Red Light Therapy Work? Science Explained
Does Red Light Therapy Work? What Science, Doctors, and Real-World Results Say
Short answer: Yes—red light therapy works, but how well it works depends on the wavelengths used, treatment consistency, power output, and the condition being treated.
Red light therapy (also called photobiomodulation) has moved from research labs into hospitals, physical therapy clinics, dermatology offices, and now homes—thanks to advancements in LED technology. Major medical publishers like WebMD now recognize it as a legitimate, research-supported therapy for skin health, pain, inflammation, and recovery.
This guide explains what red light therapy actually does, what science supports it, who benefits most, and how to use it correctly—so you can decide if it’s worth adding to your wellness routine.
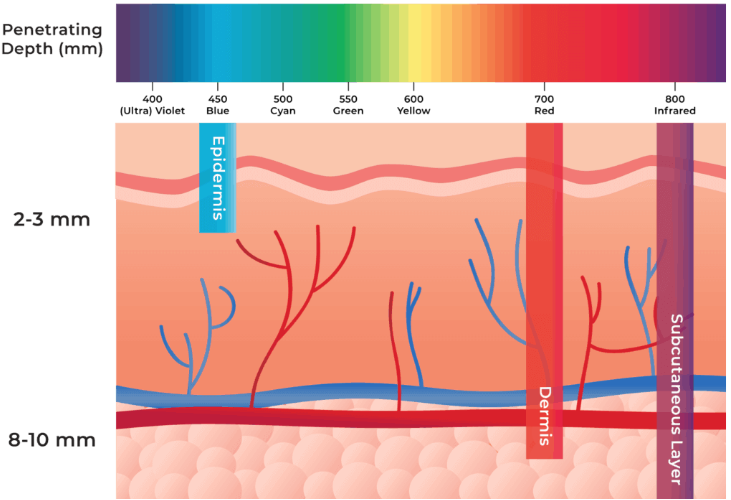
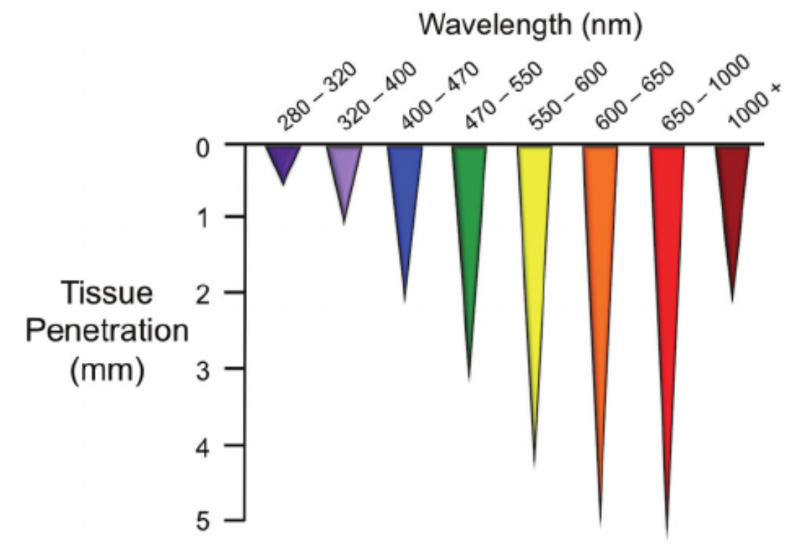
Red light therapy uses specific wavelengths of visible red light (typically ~630–660 nm) and near-infrared light (~810–880 nm) to stimulate biological processes inside the body.
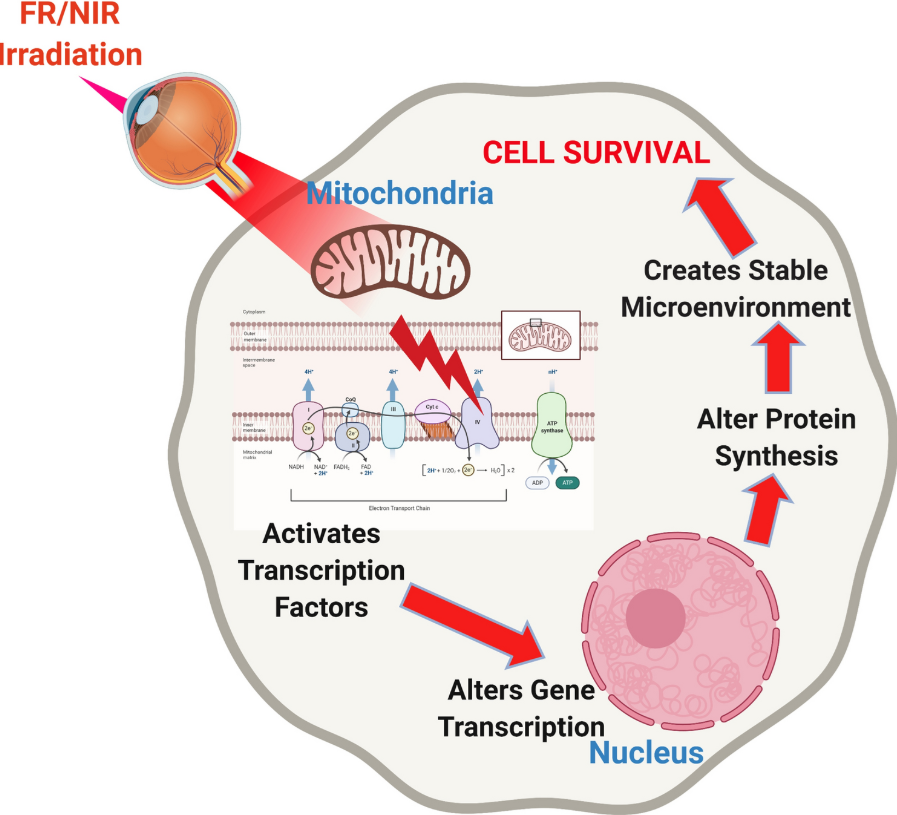
Unlike UV light, red and near-infrared light do not damage DNA or burn skin. Instead, they penetrate tissue and interact with mitochondria—the energy centers of your cells.
At the cellular level, red light therapy helps:
Increase ATP (cellular energy)
Improve blood flow and oxygenation
Reduce inflammation
Support tissue repair
Modulate oxidative stress
This is why it’s used across dermatology, physical therapy, sports medicine, and pain management.
What Does the Medical Evidence Say?
According to medical summaries like those published by WebMD, red light therapy has moderate to strong evidence for several applications—particularly when used consistently and at therapeutic power levels.
Areas with the strongest scientific support:
1. Skin Health & Anti-Aging
Research supports improvements in:
Fine lines and wrinkles
Skin texture and tone
Collagen and elastin production
Acne inflammation (not bacterial killing)
2. Pain & Inflammation
Clinical studies show benefits for:
Joint pain and stiffness
Muscle soreness
Arthritis-related discomfort
Tendon and soft-tissue irritation
3. Muscle Recovery & Performance
Used by physical therapists and athletes to:
Speed post-exercise recovery
Reduce delayed-onset muscle soreness (DOMS)
Improve local circulation
4. Wound Healing & Tissue Repair
Medical-grade photobiomodulation has been used in:
Post-surgical recovery
Chronic wounds
Scar remodeling
Does Red Light Therapy Work for Everyone?
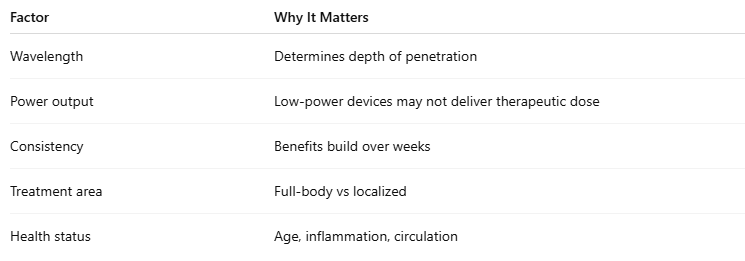
Red light therapy is not a miracle cure, and results vary based on:
Most people who follow proper protocols notice:
Improved skin appearance in 4–8 weeks
Reduced soreness within days to weeks
Gradual improvements in energy and recovery
Is Red Light Therapy Safe?
For most healthy adults, red light therapy is considered very safe when used correctly.
Safety considerations:
Non-invasive
No UV radiation
No known long-term tissue damage
Minimal side effects (temporary warmth or redness)
Consult a healthcare provider if you:
Are pregnant
Have active cancer
Take photosensitizing medications
Have light-sensitive conditions
Why Device Quality Matters (This Is Where Results Change)
One of the biggest reasons people say “red light therapy didn’t work” is underpowered devices.
Therapeutic results require:
Correct wavelengths (red + near-infrared)
Adequate irradiance (power density)
Enough coverage area
Proper exposure time
This is why clinical-grade LED panels outperform:
Small handheld gadgets
Beauty-only masks
Low-power consumer lights
Why a Red Light Therapy Panel Works Better Than Small Devices
A high-quality red light therapy panel provides:
✔ Full-body coverage
✔ Deeper tissue penetration
✔ Consistent therapeutic dosing
✔ Better long-term value
✔ Clinic-level output at home
Panels are ideal for:
Pain relief
Recovery
Skin health
Energy and wellness routines
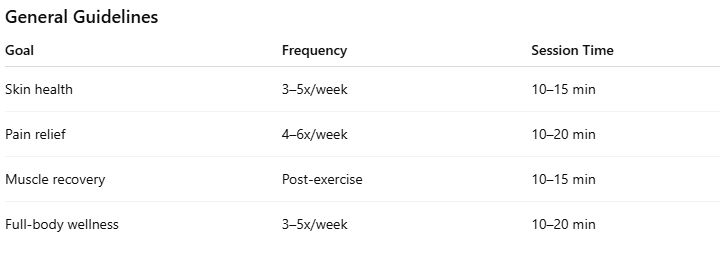
How to Use Red Light Therapy for Best Results
Bottom Line: Consistency matters more than intensity.
Does Red Light Therapy Actually Work Long-Term?
When used correctly:
Benefits accumulate, not disappear
Many users integrate it into daily routines
Long-term users often reduce reliance on pain meds or cosmetic procedures
Red light therapy works best as a supportive wellness tool, not a standalone medical treatment.
Ready to Experience Real Results?
👉 Shop Our Clinical-Grade Red Light Therapy Panels
Perfect for skin, pain relief, recovery, and total wellness.
Start Your Red Light Therapy Journey → Get Your Own Red Light Panel Here
FAQ
Does red light therapy really work?
Yes—when proper wavelengths, power output, and consistency are used.
Is red light therapy FDA approved?
Some devices are FDA-cleared for specific uses like pain and skin treatment.
How long before I see results?
Some benefits appear within weeks; others build over months.
More from Medford Red Light Therapy: Check out our most popular blogs on red light therapy to save you time and money on your next purchase with Medford Red Light Therapy:
Scientific References:
Karu TI, Pyatibrat LV, Kalendo GS. Photobiological modulation of cell attachment via cytochrome c oxidase. Photochem Photobiol Sci. 2004 Feb;3(2):211–216.
Oron U. Light therapy and stem cells: a therapeutic intervention of the future? Interventional Cardiology. 2011;3(6):627–629.
Lane N. Cell biology: power games. Nature. 2006 Oct 26;443(7114):901–903.
Karu T. Primary and secondary mechanisms of action of visible to near-IR radiation on cells. J Photochem Photobiol B. 1999 Mar;49(1):1–17.
Liu H, Colavitti R, Rovira, Finkel T. Redox-dependent transcriptional regulation. Circ Res. 2005 Nov 11;97(10):967–974.
Huang YY, Chen AC, Carroll JD, Hamblin MR. Biphasic dose response in low level light therapy. Dose Response. 2009;7(4):358–383.
Pastore D, Greco M, Petragallo VA, Passarella S. Increase in <--H+/e- ratio of the cytochrome c oxidase reaction in mitochondria irradiated with helium-neon laser. Biochem Mol Biol Int. 1994 Oct;34(4):817–826.
Karu T, Pyatibrat L, Kalendo G. Irradiation with He-Ne laser increases ATP level in cells cultivated in vitro. J Photochem Photobiol B. 1995 Mar;27(3):219–223.
AlGhamdi KM, Kumar A, Moussa NA. Low-level laser therapy: a useful technique for enhancing the proliferation of various cultured cells. Lasers Med Sci. 2012 Jan;27(1):237–249.
Hode L. The importance of the coherency. Photomed Laser Surg. 2005 Aug;23(4):431–434.
Wong-Riley MT, Liang HL, Eells JT, et al. Photobiomodulation directly benefits primary neurons functionally inactivated by toxins: role of cytochrome c oxidase. J Biol Chem. 2005 Feb 11;280(6):4761–4771.
Basford JR. Low intensity laser therapy: still not an established clinical tool. Lasers Surg Med. 1995;16(4):331–342.
Posten W, Wrone DA, Dover JS, Arndt KA, Silapunt S, Alam M. Low-level laser therapy for wound healing: mechanism and efficacy. Dermatol Surg. 2005 Mar;31(3):334–340.
Huang YY, Sharma SK, Carroll J, Hamblin MR. Biphasic dose response in low level light therapy - an update. Dose Response. 2011;9(4):602–618.
Paasch U, Haedersdal M. Laser systems for ablative fractional resurfacing. Expert Rev Med Devices. 2011 Jan;8(1):67–83.
Weiss RA, McDaniel DH, Geronemus RG. Review of nonablative photorejuvenation: reversal of the aging effects of the sun and environmental damage using laser and light sources. Semin Cutan Med Surg. 2003 Jun;22(2):93–106.
Peplow PV, Chung TY, Ryan B, Baxter GD. Laser photobiomodulation of gene expression and release of growth factors and cytokines from cells in culture: a review of human and animal studies. Photomed Laser Surg. 2011 May;29(5):285–304.
Lee SY, Park KH, Choi JW, et al. A prospective, randomized, placebo-controlled, double-blinded, and split-face clinical study on LED phototherapy for skin rejuvenation: clinical, profilometric, histologic, ultrastructural, and biochemical evaluations and comparison of three different treatment settings. J Photochem Photobiol B. 2007 Jul 27;88(1):51–67.
Nanni CA, Alster TS. Complications of carbon dioxide laser resurfacing. An evaluation of 500 patients. Dermatol Surg. 1998 Mar;24(3):315–320.
Sachdev M, Hameed S, Mysore V. Nonablative lasers and nonlaser systems in dermatology: current status. Indian J Dermatol Venereol Leprol. 2011 May-Jun;77(3):380–388.
Dierickx CC, Anderson RR. Visible light treatment of photoaging. Dermatol Ther. 2005 May-Jun;18(3):191–208.
Hardaway CA, Ross EV. Nonablative laser skin remodeling. Dermatol Clin. 2002 Jan;20(1):97–111. ix.
Sriprachya-Anunt S, Fitzpatrick RE, Goldman MP, Smith SR. Infections complicating pulsed carbon dioxide laser resurfacing for photoaged facial skin. Dermatol Surg. 1997 Jul;23(7):527–535. discussion 535–526.
Weiss RA, McDaniel DH, Geronemus RG, et al. Clinical experience with light-emitting diode (LED) photomodulation. Dermatol Surg. 2005 Sep;31(9 Pt 2):1199–1205.
Barolet D, Roberge CJ, Auger FA, Boucher A, Germain L. Regulation of skin collagen metabolism in vitro using a pulsed 660 nm LED light source: clinical correlation with a single-blinded study. J Invest Dermatol. 2009 Dec;129(12):2751–2759.
Abergel RP, Lyons RF, Castel JC, Dwyer RM, Uitto J. Biostimulation of wound healing by lasers: experimental approaches in animal models and in fibroblast cultures. J Dermatol Surg Oncol. 1987 Feb;13(2):127–133.
Russell BA, Kellett N, Reilly LR. A study to determine the efficacy of combination LED light therapy (633 nm and 830 nm) in facial skin rejuvenation. J Cosmet Laser Ther. 2005 Dec;7(3–4):196–200.
Weiss RA, McDaniel DH, Geronemus RG, Weiss MA. Clinical trial of a novel nonthermal LED array for reversal of photoaging: clinical, histologic, and surface profilometric results. Lasers Surg Med. 2005 Feb;36(2):85–91.
Bhat J, Birch J, Whitehurst C, Lanigan SW. A single-blinded randomised controlled study to determine the efficacy of Omnilux Revive facial treatment in skin rejuvenation. Lasers Med Sci. 2005;20(1):6–10.
Weiss RA, Weiss MA, Geronemus RG, McDaniel DH. A novel non-thermal non-ablative full panel LED photomodulation device for reversal of photoaging: digital microscopic and clinical results in various skin types. J Drugs Dermatol. 2004 Nov-Dec;3(6):605–610.
McDaniel DH, Newman J, Geronemus R, et al. Non-ablative non- thermal LED photomodulation—a multicenter clinical photoaging trial. Lasers Surg Med. 2003;15:22.
Yu W, Naim JO, Lanzafame RJ. The effect of laser irradiation on the release of bFGF from 3T3 fibroblasts. Photochem Photobiol. 1994 Feb;59(2):167–170.
Kucuk BB, Oral K, Selcuk NA, Toklu T, Civi OG. The anti-inflammatory effect of low-level laser therapy on experimentally induced inflammation of rabbit temporomandibular joint retrodiscal tissues. J Orofac Pain. 2010 Summer;24(3):293–297.
Geronemus RG, Weiss RA, Weiss MA, et al. Non-ablative LED photomodulation light activated fibroblast stimulation clinical trial. Lasers Surg Med. 2003;25:22.
Schindl A, Heinze G, Schindl M, Pernerstorfer-Schon H, Schindl L. Systemic effects of low-intensity laser irradiation on skin microcirculation in patients with diabetic microangiopathy. Microvasc Res. 2002 Sep;64(2):240–246.
Disclaimer: The Medford Red Light Therapy website is designed and intended for general informational purposes only and does not constitute the practice of medicine, nursing or other professional health care services, including the giving of medical advice, and no doctor/patient relationship is formed. The use of information on this website is at the user’s own risk. Results may vary by individual. The content of this website is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Users should not disregard or delay in obtaining medical advice for any medical condition they may have and should seek the assistance of their health care professionals for any such conditions.